Men's Health
Men's Health Physiotherapy
Sycamore Health offers services for men’s health conditions. Problems such as poor urinary or bowel incontinence, erectile dysfunction and pelvic pain can have a huge impact on the life of men, limiting engagement in social activities, relationships, maintaining health, mental health and work. These conditions are highly treatable and with the appropriate strategies, you can make positive changes, manage and improve your condition. We know men can be silent sufferers with these problems and we needn’t be - as blokes, we aim to provide a safe space to discuss these issues and more to make a meaningful difference in your life with quality treatment.
Who might need men’s health physiotherapy?
If you experience symptoms such as the following, you may benefit from engaging in men’s health physiotherapy treatment:
- Leaking urine with coughing, sneezing or lifting
- Suffering from frequent, strong urges to pee
- Increased frequency of urination, sometimes needing to go and little urine being voided
- Interrupted flow of urine - difficulty starting or stopping
- Leaking/dribbling after urination
- Difficulty controlling your bowels
- Those undergoing prostate cancer treatment (pre & post op)
- Suffering from erectile dysfunction
- Pain with erections or orgasms
- Acute and chronic pelvic region pain
Prostate Cancer
Continence problems after prostate surgery are common and an expected side effect to treatment. We’re there to help support you through this challenging time in your life. Seeing a men’s health physiotherapist can help you regain control of your bladder much faster and help guide you post operatively with returning to work, your hobbies and exercise.
What does a men’s health physiotherapy appointment look like?
A men’s health consultation will include a good chat to gather information about your condition (the exact problem you are experiencing, deep diving into your symptoms, how long it’s been going on, etc.), getting a thorough medical history, discussing things which might be contributing to your condition and areas we might be able to address (such as a diet, fluid intake, exercise), gaining an understanding of your life (what you like to do, your work, relationships, hobbies, etc.) and how your condition is making an impact in your life so treatment can best be tailored to suit you.
From there we will go on to an objective assessment to gain further insight into understanding your problem. This often includes assessment of your pelvic floor muscle function. We have access to real time ultrasound which allows us to get a real time image of how your pelvic floor muscles are functioning, your ability to actively control their contractions, their endurance and strength. If indicated, a neurological screen and a movement exam will be conducted. We also use questionnaires and diaries to assess urinary and bowel habits which may be playing a part in the problem condition.
With our assessment findings, we will work with you to devise a treatment plan. This will likely entail an exercise program to train your pelvic floor muscles. We will discuss strategies to manage your condition to lessen its impact on your life in the meantime whilst we work towards resolution. We will work together to create a holistic plan to improve your general well-being - healthy lifestyle changes, general exercise, diet, assistance with engaging in support groups where needed. Creating a safe space to discuss any issues which may be arising due to the impact of your condition.
Men’s Health at Sycamore Health
Tackling these health problems can be challenging, they’re difficult to talk about and can cause large disruptions to how you want to live your life. At Sycamore Health, we’re committed to providing the highest quality holistic treatment. We’re blokes supporting blokes, here to walk with you through your health journey, offering support, professional advice and treatment to help you get on top of your condition and return to life.
Why choose Sycamore Health?
Two Convenient Locations in Morayfield and Sippy Downs: our clinics are ideally located in the heart of Morayfield and Sippy Downs.
Easy online bookings: we offer a straight-forward online booking system so that you can book your appointment in seconds, no matter the time of day.
Same-day appointments: we understand that sometimes you need to be seen by our team as soon as possible, so we keep a number of appointments each day for those who need help urgently.
Private treatment rooms: our treatment is provided one-on-one in private rooms to make sure you are comfortable.
A range of physiotherapy services: we offer a range of physiotherapy services, including hands-on treatment, custom home exercise programs, gym-based rehabilitation and tailored advice.
Qualified, highly-trained physiotherapists: our team of physiotherapists are all highly-skilled and fully qualified.
Customised therapies: we know that your situation is unique and will tailor your program and exercises to suit you.
Prostate Cancer
Men's health physiotherapists are trained in helping you manage with a diagnosis of prostate cancer. They can manage symptoms such as urinary and faecal incontinence, voiding pain and difficulty, erectile dysfunction and more. Our expert physiotherapists can help with your pre and post-surgical rehabilitation.
The prostate is a gland that sits just below the bladder in men. It is about the size of a walnut and surrounds the urethra (the tube which your urine passes through as it leaves the bladder) and plays an important role in fertility. It produces seminal fluid which contains enzymes, zinc, citrate and fructose which helps sperm survive within the fluid.
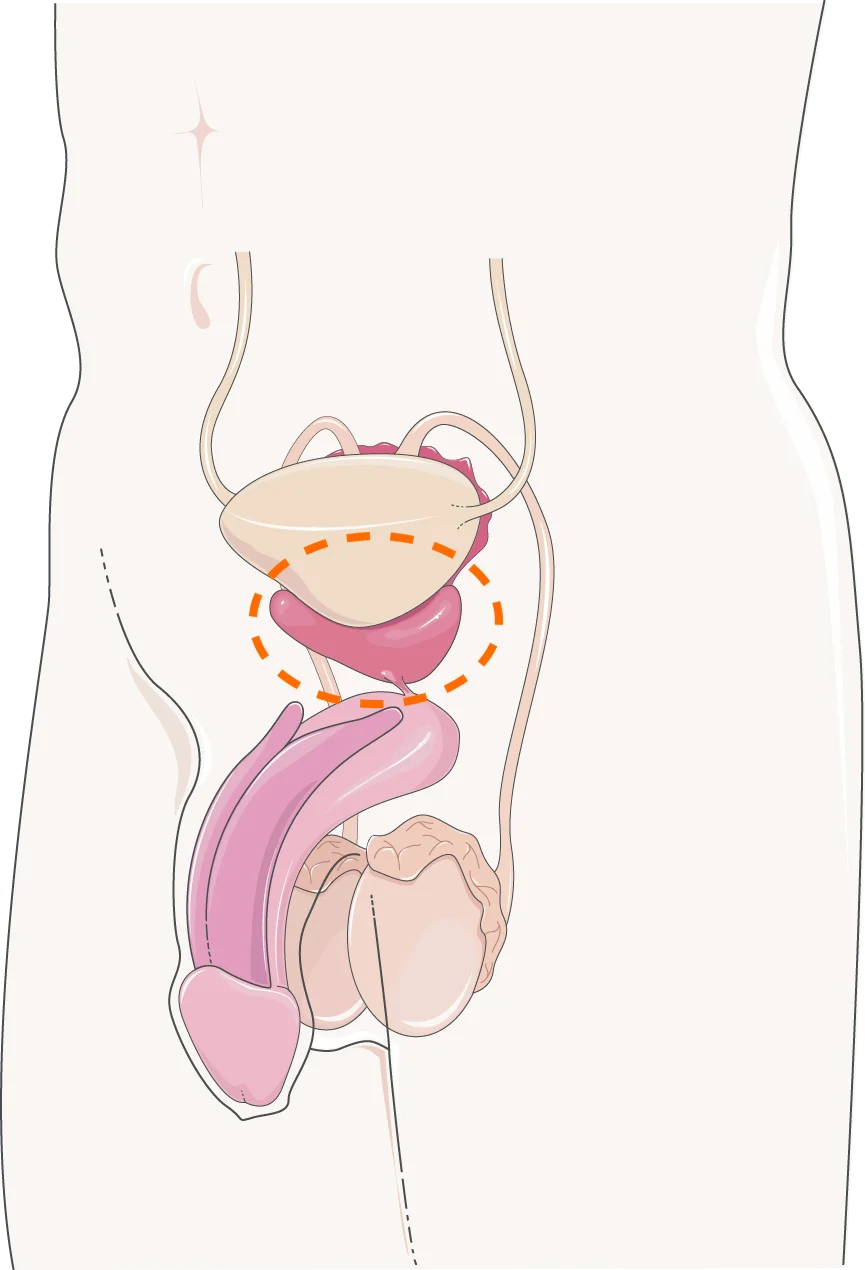
The prostate is located underneath the bladder
Age: Increasing age is the main risk factor for prostate cancer. For white men with no family history, the risk for getting prostate cancer increases significantly after the age of 50. This is why routine screening investigations are recommended from age 50 onwards.
Family history: Having a close relative diagnosed with prostate cancer is another risk factor. Having multiple relatives diagnosed (such as a brother and a father) further increases this risk. Risk is further increased if those relatives were diagnosed at a younger age. The increased risk has been reported to be up to 2.3 fold increased likelihood of a prostate cancer diagnosis.
Several lifestyle factors have been identified as modifiable risk factors associated with prostate cancer development and prognosis such as smoking and physical activity. Smoking cessation and engaging in physical activity has shown to have positive impacts on reducing the risk of developing prostate cancer and improving outcomes with a prostate cancer diagnosis.
Urinary symptoms are the most typical symptoms one may experience with prostate cancer and include:
- Weakened flow whilst urinating
- Difficulty commencing urination
- Painful urination
- Difficulty fully emptying the bladder
- Increased frequency of urination
Sexual dysfunction:
- Painful orgasm/ejaculation
- Difficulty achieving or maintaining erection
Many men can also be asymptomatic.
A PSA test (prostate specific antigen) and/or a DRE (digital rectal examination) are used to routinely screen for prostate cancer. Elevated PSA indicates an increased risk of prostate cancer, however, is not definitive as there are other factors which may increase PSA levels. A medical practitioner may perform a DRE in conjunction to feel for abnormalities of the prostate.
If prostate cancer is suspected with the above screening tests, a biopsy will usually be done. This involves taking a part of the prostate tissue and examining it under a microscope for cancerous cells. This is the only way in which prostate cancer can be confirmed.
There are two main treatment options for prostate cancer. Each having varying side effects.
- Surgery (prostatectomy): This involves removal of the whole prostate gland.
- Radiation: This involves targeted radiation at the cancerous cells in the prostate gland
Surgery
- Incontinence: Most men have urinary incontinence initially after surgery, however this can and typically recovers over time and with physiotherapy. Due to its proximity to the prostate, the removal of the internal urinary sphincter is necessary. This is one of our muscles we rely on to maintain our continence. It is under involuntary control, meaning it requires no active thought from the brain to make it contract and acts to constrict the urethra preventing the flow of urine. After its removal during the surgery, we need to rely on other pelvic floor muscles to compensate for this. Our pelvic floor muscles play an important role in helping us control our bladder.
- Sexual dysfunction: Prostatectomy can also result in changes in sexual function. This can include problems with erections, pain with orgasm, difficulty reaching orgasm and decreased sensation. A nerve called the cavernous nerve supplies the penis and is responsible for sexual function and being able to achieve erections. Due to the proximity of the cavernous nerves to the prostate, they are impacted during surgery. These nerves form a bundle which surrounds the prostate gland and can be spared during the operation. However, during the procedure they are moved out of the way and become ‘shocked’, losing their function due to the irritation. Over time and with stimulation of these nerves, there is potential for recovery.
- Penile shortening - as the prostate is removed so is the portion of the urethra that passes through it - the urethra is then attached at the bladder neck, shortening it. Over time, the bladder drops down, lengthening the portion of the urethra external to the body.
- Side effects with radiation are similar to that one would experience with surgery, however, there are a few differences. Typically side effects from radiation therapy will occur later, about between two and five years. This is due to radiation destroying the cancerous and surrounding prostate tissue over time rather than immediately as occurs in surgery.
- Incontinence: Incontinence is a common side effect with radiation as well, however, the type of incontinence is varied. With radiation, urge incontinence is predominant versus stress incontinence. Urge incontinence is where the communication between the bladder and the brain is compromised causing extremely strong urges to pee when the bladder isn’t full, and frequent urination which can be very disruptive to our daily lives.
Radiation
Physiotherapy with prostate cancer focuses on optimising outcomes with urinary and sexual dysfunction post operatively. This largely consists of pelvic floor muscle training exercises in order to re-train them to function properly. With the removal of the internal urinary sphincter, we must train the brain to activate other pelvic floor muscles to contract to help us remain continent. A physiotherapist will help guide you in how to achieve this and provide feedback on how you are going with training this.
It is also valuable to see a physiotherapist for education around what to expect before and after your surgery. Having a good understanding of this can help set you up for success. This stuff can be hard to talk about. Having a physiotherapist whom you see regularly and have a good rapport with can help provide a space for you to discuss these sensitive topics.
Lifestyle changes such as weight loss, improving your diet and engaging in a regular exercise program can help improve your outcomes with prostate cancer. A physiotherapist can also help guide you here.
Most men will recover continence within 6-9 months after prostatectomy. At 12 months, about 90% of men usually have recovered their continence. These are general timeframes, and each person is unique. Consult with your urologist, general practitioner and physiotherapist to gain a fuller understanding of your recovery timeframe.
Erectile function can take a while to recover - usually between 12 and 24 months. Nerves are very sensitive and recover slowly. The impact from the ‘shock’ during surgery means it takes a significant amount of time for their function to be restored. The change to your ability to obtain and sustain arrousal can be quite confronting. Undoubtedly, this will have a large impact on your sexual life. Yet, it's important to navigate this part of your recovery in an open and intentional way, seeking the guidance of your physiotherapist, and medical professionals. There are many ways to improve the odds of you having a full sexual recovery after prostatectomy, starting as early as a few weeks post-operatively.

Overactive Bladder
Our pelvic floor physiotherapists are trained to manage the signs and symptoms of OAB.
Overactive bladder (OAB) is a condition characterised by involuntary contractions of the bladder muscles (detrusor muscle). The bladder is controlled by a complex network of nerves and muscles that work together to store and release urine. When the bladder is full, receptors which detect stretch of the bladder wall send nerve signals to the brain, which interprets the signals as the need to urinate. In individuals with OAB, this detection/signaling process can become disrupted, leading to a sensation of urgency even when the bladder isn’t full and an increased frequency of urination.
Symptoms of OAB in men may include sudden, intense urges to urinate that cannot be delayed, high frequency of urination (eight or more times per day), waking up at night to urinate (nocturia), and urge urinary incontinence (having such a strong urge to pee that some urine is leaked).
OAB can have significant impacts on the lives of those experiencing the symptoms from it. It can be extremely limiting in social situations, making people avoid engaging in interactions due to fear of leaking or embarrassment. It can be restrictive for people to be able to engage in healthy habits such as exercise. Often people suffering from OAB will have their daily lives, routines and movements dictated by their symptoms such as planning out where they go based on availability of toilets, limiting variety of areas they go where they go due to familiarity of where bathrooms are located, peeing (or trying to) before every activity or going out.
Overactive bladder affects about 11.8% of men aged 40 years or more. This prevalence increases with age , affecting 7.9% in men aged 40-49 years, 13.7% in men aged 50-59 years, 16.6% in men aged 60-69 years, and 20.3% in men aged 70 years and older.
Overactive bladder is a clinical diagnosis, meaning it is diagnosed based on the symptoms of the condition outlined above. Other tests may be performed to rule out other potential causes of the same symptoms such as urinalysis to rule out urinary tract infection. Once these are ruled out, a diagnosis of OAB can be made.
Other tests which may be performed are urodynamic tests (obtaining measures of flow & pressures), Post-void residual volume (PVR) to measure urine left in the bladder after urinating and bladder dairy (measuring frequency and volume of voids across a (usually) 3 day period).
Physiotherapy can help with the management of overactive bladder using a few different methods, used in conjunction with each other. These involve pelvic floor muscle training, bladder retraining & optimising lifestyle factors which negatively impact OAB.
A men’s health physiotherapist will help walk with you along your rehabilitation journey with your OAB symptoms to help with progression as you conquer these symptoms, to aid when you have setbacks (which are likely) and provide guidance on managing day to day with OAB symptoms.
Bladder training is a process by which we retrain the communication between the bladder and the brain to restore normal signalling that the bladder is full. This involves gradually increasing time between visits to the bathroom either by sticking to a set schedule & slowly extending the duration between bathroom visits or by deferring bathroom visits when you get urges. This helps ‘stretch’, or rather, improve the bladder's tolerability to stretch and how soon it signals to the brain that it is full.
Distraction and relaxation techniques can be used to help reduce the intensity of urges during the training process.
It will likely take several months to overcome the effects of overactive bladder. It can take some time to improve strength & control of pelvic floor muscles and improve the communication of nerve signalling between the bladder and the brain.

Pelvic Floor
Mens health physiotherapy work specifically to help strengthen and train your pelvic floor. Often, the pelvic floor is ignored, yet it contributes to a significant number of urinary, faecal and sexual functions in the body.
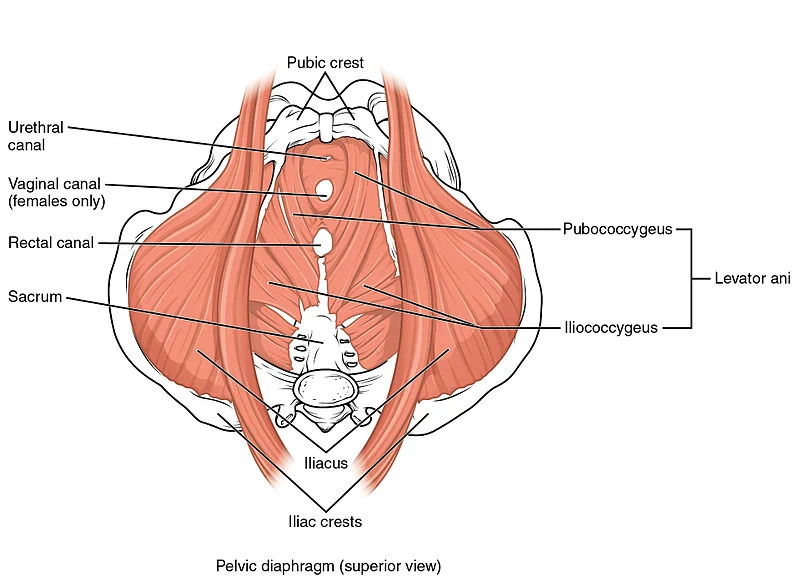
The pelvic floor is a group of muscles that stretch from the tailbone to the pubic bone (from the back to the front of the base of the pelvis) and support the pelvic organs, including the bladder, rectum, and prostate gland in men. These muscles are made up of three layers: the superficial layer, the middle layer and the deep layer. The superficial layer is composed of the bulbospongiosus, ischiocavernosus, and transverse perineal muscles which are involved in urinary and faecal continence as well as playing a role in ejaculation. The middle layer consists of the deep transverse perineal muscles and the perineal membrane. The deep layer includes the puborectalis, pubococcygeus, and iliococcygeus muscles and is involved in the maintenance of continence and supporting the internal organs.
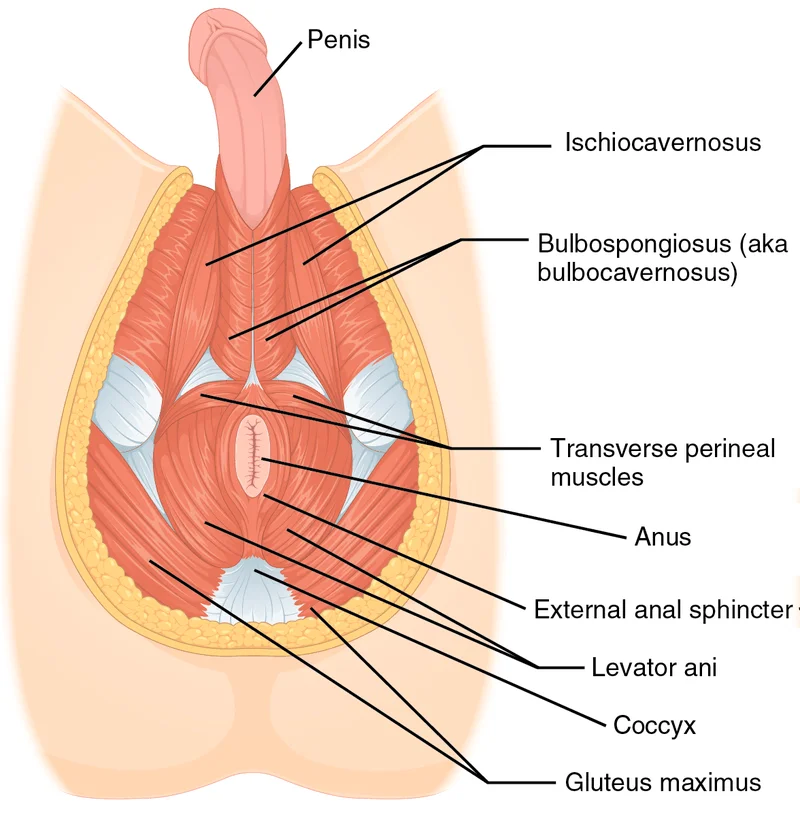
The pelvic floor muscles contribute to continence by acting as a sling or hammock, supporting the pelvic organs and maintaining their proper position. The muscles are responsible for controlling the urethral and anal sphincters, which allow for voluntary control of urination and defecation. When the pelvic floor muscles are weak or dysfunctional, it can lead to incontinence (an inability to control voluntary function of bladder or bowel movements leading to leakage of urine or stool). The pelvic floor muscles also physically support the bladder and bowels, helping maintain the correct pressure within the bladder. Additionally, the pelvic floor muscles are involved in sexual function, including maintaining an erection in men and orgasm in both men and women.
The pelvic floor muscles contribute to maintaining our continence as they surround the urethra (the tube that carries urine from our bladder out of our body) and the rectum (the passageway from our intestines out of our body). By surrounding these structures, when these muscles contract, they squeeze around these tubes, constricting them and disallowing the passing urine or faeces. We can control this, and conversely (hopefully when we’re at the appropriate place to urinate or defecate) when these muscles relax, they allow urine or stool to be released. The strength & coordination of these muscles are key factors in being able to maintain our control of this function, thus our continence.
The pelvic floor can become dysfunctional and the pelvic floor muscles can become weak, tight, or have poor coordination, leading to a range of symptoms, most typically incontinence by not being able to control the constriction of the urethra and rectum as outlined above. Other symptoms can include erectile dysfunction, painful urination or bowel movements, and pain or discomfort in the pelvic area.
There are a few factors that can contribute to dysfunction of the pelvic floor muscles. Undergoing prostate surgery is one of the primary reasons men experience pelvic floor dysfunction. It is thought this may be due to: a disruption in neural function supplying the pelvic floor muscles; inflammation in the area of the prostate due to the surgery; a change in the position of the pelvic organs with the removal of the prostate gland; a change in bladder function after surgery.
- Increases in age
- Chronic coughing - every time you cough, the pressure within your abdominal cavity increases putting pressure on the bladder, the pelvic floor muscles contract to constrict the urethra to prevent urine flow. Coughing lots for a long time can lead to strain and tension within these muscles.
- Chronic constipation can lead to strain and tension within the pelvic floor muscles
- Obesity can increase the demand on the pelvic floor muscles, leading to fatigue and weakness
Pelvic floor muscle training (PFMT) is a great tool to help overcome challenges you may have with dysfunction and improve your continence. Just like any other muscle, your pelvic floor can be trained! It can be tricky though as you can’t see your pelvic floor, thus it’s hard to get feedback on whether you’re performing the exercise correctly. This pelvic floor muscle training can help improve the strength and endurance of these muscles but most importantly your control of these muscles (the ability for your brain to signal to these muscles to contract).
It is important to learn to isolate and contract the pelvic floor for pelvic floor training. Using cues is most helpful to achieve this. Cues such as ‘nuts to guts’ or ‘stopping the flow of urine’ or ‘shortening the length of your penis’ are helpful for most men trying to contract these muscles. It is important to ensure the contraction is localised to just the pelvic floor (the rest of your body should be relaxed - don’t hold your breath or contract your abdominals!). A physiotherapist can help guide you through this and ensure you are performing the exercises correctly.
Often it is recommended to use various types of contractions to train your pelvic floor in different ways. Your muscles have two different types of fibres called slow twitch and fast twitch fibres. Slow twitch fibres are better for endurance (think contracting all day to support your organs and provide light pressure to the urethra to prevent leaking) and fast twitch fibres are better for contracting quickly and forcefully (think preventing leaking when you cough, run or jump). Therefore it’s best to practice holding a light contraction for a few seconds before releasing and fully relaxing (this is important) the pelvic floor and slowly increasing the time you can hold it. To train the fast twitch fibres you can do what is called ‘the knack’ ('ma ma ma myyy Sharona! ... no, not that Knack - but if that helps you remember it, great!). This is a fast, strong, well timed contraction held briefly, then fully relaxed.
At Sycamore Health, we have expert physiotherapists who have undergone additional training in the area of Men’s Health. We can provide a thorough assessment of your pelvic floor function and work with you to regain control of your continence and your life. We will work with you to ensure you are able to perform the exercises properly and have the correct prescription. We have access to real time ultrasound which can be a very effective tool to get live feedback of your pelvic floor function and your ability to control it.
Make an enquiry with our lovely reception staff on (07) 2102 3855, or email info@sycamorehealth.com.au. Otherwise, if you're ready to book, book online here.

Erectile Dysfunction
Mens health physiotherapy work specifically to help you understand the origin of your Erectile Dysfunction (ED). Physiotherapy can help to improve erection strength, duration and function. ED is complex, with multiple possible contributing sources. Getting the right guidance is important to getting the right solution.
Erectile dysfunction (ED) is difficulty having or maintaining an erection that is sufficient for satisfying sexual activity. It can be caused by a variety of underlying problems, such as neurological changes, vascular changes or psychosocial changes. It can affect men of all ages, but it becomes more prevalent with increasing age. ED is common after certain procedures, such as prostatectomy surgery, or hormone suppression therapy. ED can be transient, meaning it will improve, or it can be permanent. Everyone who has ED, experiences it differently. It doesn't have to be a sexual 'death sentence'.

- Physical causes: Conditions such as uncontrolled diabetes, high blood pressure, heart disease, obesity, hormonal imbalances, surgeries (such as prostatectomy) and certain medications can contribute to ED.
- Psychological causes: Stress, anxiety, depression, relationship problems, and performance anxiety can all play a role in causing or exacerbating ED.
- Lifestyle factors: Unhealthy habits like smoking, excessive alcohol consumption, drug use, and lack of exercise can also contribute to ED.
While ED cannot always be prevented, certain lifestyle choices can reduce the risk. Remember the 'causes' are multifactoral, which gives you a lot of areas to work with that are under your control. For example, maintaining a healthy weight, exercising regularly, eating a balanced diet, managing stress, and avoiding substance abuse can help promote erectile function. However, how a prostatectomy surgery is performed (nerve sparing or not) is less in your control. Certain levels of cancer increase the risk of developing ED after cancer treatment. It's important not to disparage yourself if you do develop ED.
Regular check-ups with your General Practitioner are important for monitoring overall health and addressing any potential issues promptly.
Penile pumps, also known as vacuum erection devices (VEDs), are non-invasive devices designed to help improve erectile function in men with Erectile Dysfunction (ED). Here's an explanation of how they work:
Device Structure: A penile pump typically consists of a plastic cylinder that fits over the penis, a manual or battery-operated pump, and a constriction ring or band.
Creating Vacuum: To use a penile pump, the cylinder is placed over the flaccid penis. The pump is then used to create a vacuum inside the cylinder, which draws blood into the penis.
Blood Flow: As the vacuum is created, it causes blood vessels in the penis to expand and fill with blood. This increased blood flow helps to engorge the penis, resulting in an erection.
Maintaining Erection: Once an erection is achieved, a constriction ring or band is slid from the cylinder to the base of the penis. This ring helps to maintain the erection by trapping the blood within the penis and preventing it from flowing back too quickly.
Duration of Use: The recommended duration for using a penile pump may vary, but it is typically around 10 to 30 minutes. It is important to follow the instructions provided with the specific device and consult a healthcare professional if you have any concerns.
Potential Benefits: Penile pumps can be beneficial for some individuals with ED. They can provide a non-medication, non-surgical option for achieving and maintaining an erection. They can also be used as part of a comprehensive treatment plan for ED or as an alternative when other treatments are not suitable or preferred.
It's important to note that while penile pumps can be effective for some individuals, they may not be suitable for everyone. It is recommended to consult with a healthcare professional who can provide guidance on the appropriate use of a penile pump and determine if it is a suitable option for your specific situation.
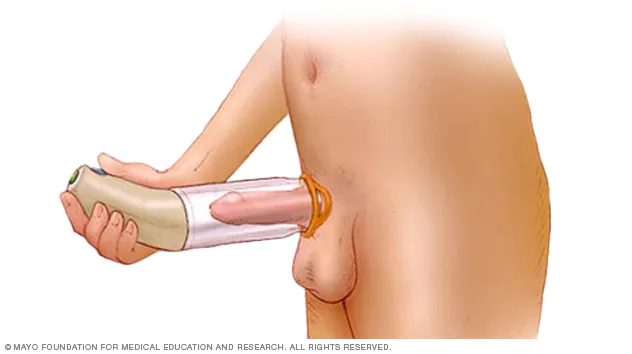
credit: mayoclinic
- There is a strong relationship to the function of the pelvic floor and erectile function. Improving your pelvic floor muscle control/strength: A physiotherapist can help guide you through retaining a group of muscles called your pelvic floor. This group of muscles are strongly involved in helping aid with urinary and faecal incontinence and can be impacted by prostate surgeries. Learn more about the pelvic floor here.
- Support through prostate cancer treatment and improving post-op outcomes: Physiotherapy intervention is important pre & post prostate cancer surgery to help regain urinary & sexual function to their greatest potential. This often involves pelvic floor muscle training for restoring continence and erectile function, education around lifestyle modification which can positively impact outcomes post operatively. Learn more about prostate cancer here.
- Men's health physiotherapists can guide you on what medical aids are appropriate for managing your ED. This may include the use of penile pumps, education around PDE5i use, therapeutic home exercise programs (HEP) and accountability.
- Some ED is complexly linked with a chronic pelvic pain syndrome (CPPS). A physiotherapist can work with you to help you gain a good understanding around the causes of your pelvic pain, which may lead to improved sexual function.
At Sycamore Health, we can help you treat and manage your pelvic condition. We will listen to your story and find out how your condition is affecting your life and other factors which may impact your recovery. Everyone is different & will require a different treatment approach dependent on each individual and their circumstances - we will make sure you are listened to as an individual and can tailor an intervention to suit you. We will ask questions to help us determine exactly what is going on and have access to real time ultrasound which can be used to assess your strength, endurance and control of your pelvic floor muscles. From there we will work with you to devise a treatment plan to help you get on top of your health.

