ITB Pain - Part 2
Written by Mitchell Robinson
This is the second of a three-part series on Iliotibial band (ITB) pain. ITB pain is common in runners - even I've had it! The good news is that this tricky injury can be managed. In Part 1, the cause/s of ITB pain were discussed. Here in Part 2, we begin our look at treatment!
This blog provides an update on the literature around the treatment of runners with ITB pain. It is not medical advice. If you have knee pain with running book in to physio here!
How do I treat my ITB pain?
Here is a brief summary of injury rehabilitation:
De-load
Re-load
Progressive over-load
Yep, I went to uni for four years when this is all they needed to tell me. (Okay, there's a little more to it, but not much).
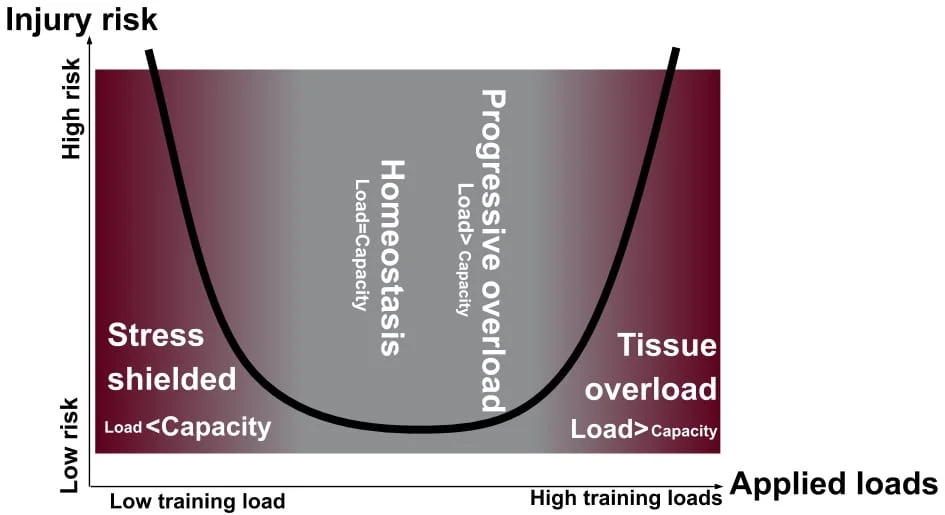
Figure 1: Tissue homeostasis model (Dye, 2005; and recently updated by Gabbett, 2016). Stress shielding is, as the name suggests, when you protect (or shield) the tissue from load (or stress) by under-loading it. Tissue overload is, as the name suggests, when you load the tissue beyond it's ability to adapt (or get stronger).
Take a minute to appreciate the figure above. There are two pitfalls to be avoided: doing too little (stress shielding) or doing too much (overload) - not rocket science I know! A well-designed rehabilitation program will aim to progressively overload the ITB to gradually restore tolerance to loads like running, weights etc. If you do too little, the chance of re-injury can be just as high as if you overload the tissue! Unfortunately, many physios and runners fall into the stress shielding trap in an effort to reduce ITB pain without actually increasing the capacity of the tissue to tolerate load. (12)
But what about foam rolling!?
We know foam rolling is very often advised for treating ITB pain, and our neglection of it is not a mistake or oversight on our part!
Here's what we know: it doesn't change flexibility for more than a few minutes (22), doesn't provide any lasting pain relief (??) and it doesn't break up or "release" adhesions in the connective tissue or myofascia.
Moreover, if ITB pain is a compression injury, then the last thing we should do is add more compression to the lateral knee!
Image 1: A hilariously accurate meme.
Well, what do I do?

Figure 2: Three main components of loads experienced by the runner. Adapted from Willy & Meira 2016.
There are three types of loads are experienced when we run and each must be appropriately addressed in a successful rehabilitation program:
- 1) peak loads (when your foot lands on the ground)
- prepared for by including heavy resistance exercises
- 2) energy storage and release (when your tissues store and release energy like a spring)
- prepared for with plyometrics
- 3) cumulative loading (accumulated over the duration of the run)
- prepared for with a graded return-to-run program (Figure 3)
Stages of Rehabilitation
There are two main stages for rehab: a pain dominant phase and a load dominant phase. These phases work on a "protect" vs. "expose" dynamic: an emphasis on "protection" to reduce pain initially, and gradually shifting the emphasis to "exposure" to build resiliency over time. These phases are motivated by previous works of Cook and Purdam (2009)(4) and Fredericson and Weir (2005)(10), which suggest keeping lateral knee pain capped at 0-4/10 visual analog scale (VAS), either during the session or upon waking the next morning.

Figure 3: Example progression of rehabilitation for a runner with ITB compression pain
Pain Dominant / "Protect" Phase
Stage 1:
The goal: maintain as much capacity as possible while avoiding irritation. This is a challenge and often requires some trial and error while you learn what you can tolerate! Running may need to be temporarily ceased or greatly reduced and replaced with other equally challenging activities that do not irritate the ITB.
During this stage uphill treadmill walking (~10% gradient) seems appropriate as it reduces knee varus moment (see Image 2), increases knee flexion at footstike helping to avoid the ITB impingement zone (~30deg knee flexion), and reduces the energy storage and release demands of the ITB.
If uphill treadmill walking is irritating, regress to stationary cycling with the seat lowered could be attempted. A possible modification may be to lower the seat such that the knee is flexed to ~35deg at the bottom of the pedal stroke (avoiding the aforementioned impingement zone).
If stationary cycling is also aggravating, regress to swimming. The goal however, is always to move towards uphill walking, even when it's not tolerated initially.
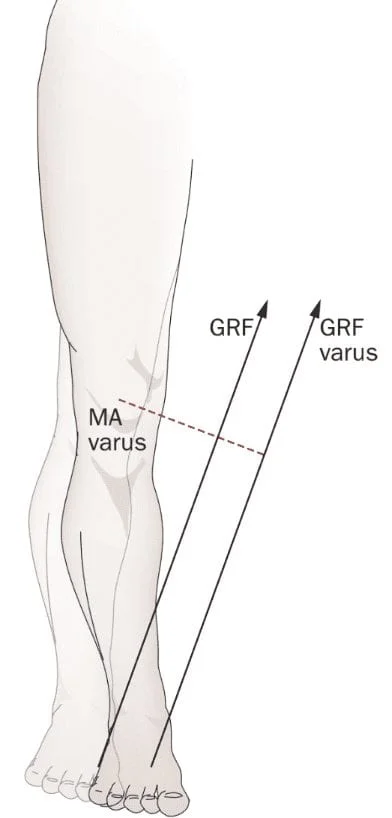
Image 2: knee varus moment arm (MA) depicted by the dotted red line. The longer this line, the larger the moment arm and the more torque applied to the knee (and hip). Uphill treadmill walking reduces the length of the moment arm thereby reducing the energy storage and release demands of the ITB during the gait cycle.
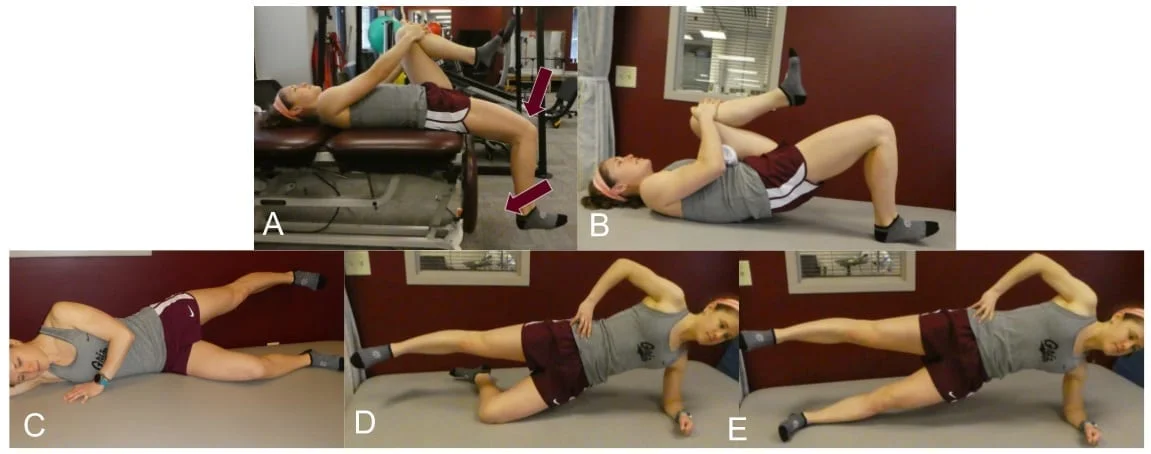
Figure 4: Stage 1 exercises. A) ITB excursion exercise (10x10” holds) progressing to (B) single leg bridge. Simultaneously, the runner is progressed through hip abductor progression (C-E).
Non-weight bearing ITB loading is initiated by progressing from A through to E above. A (basically just the Thomas Test used as an ITB excursion exercise), B (single leg bridge), C Non-weight bearing, progressive ITB and hip loading exercises are initiated in Stage 1. The ITB is loaded throughout Stage 1 via the Thomas exercise, which is really just the Thomas test used as a low-load ITB excursion exercise (Figure 4A). The Thomas exercise is then progressed to a single leg bridge (Figure 4B). Concurrent with the Thomas and single leg bridge exercises, the posterolateral hip musculature are progressively loaded (Figure 4 C-E). (20) Multiple sets of isometric holds of 10 or fewer repetitions should be prescribed with adequate hold times and efforts that achieve near-muscular failure on the last couple of repetitions.
Click here for part 3 to read our final blog in this series!
We're serious about helping you live life without pain. Right now, you can book in for a FREE initial assessment. No hidden funnies, weird pyramid schemes, or quackery. Just a great chance for you to see how physiotherapy can help you move again. In fact, we're so serious, we even offer half-price treatment should you chose to pursue your tailored therapy, right in the very same session. Press the button below to quickly make an online booking. It's no fuss and super-simple, we promise.
References:
1. Aboodarda S, Spence A, Button DC. Pain pressure threshold of a muscle tender spot increases following local and non-local rolling massage. BMC musculoskeletal disorders. 2015;16:265.
2. Boyer ER, Derrick TR. Select injury-related variables are affected by stride length and foot strike style during running. The American journal of sports medicine. 2015;43:2310-2317.
3. Chaudhry H, Schleip R, Ji Z, Bukiet B, Maney M, Findley T. Three-dimensional mathematical model for deformation of human fasciae in manual therapy. The Journal of the American Osteopathic Association. 2008;108:379-390.
4. Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med. 2009;43:409-416.
5. Davis I. Optimising the efficacy of gait retraining. BMJ Publishing Group Ltd and British Association of Sport and Exercise Medicine; 2018.
6. Dye SF. The pathophysiology of patellofemoral pain: a tissue homeostasis perspective. Clin Orthop Relat Res. 2005;100-110.
7. Fairclough J, Hayashi K, Toumi H, et al. The functional anatomy of the iliotibial band during flexion and extension of the knee: implications for understanding iliotibial band syndrome. Journal of anatomy. 2006;208:309-316.
8. Fairclough J, Hayashi K, Toumi H, et al. Is iliotibial band syndrome really a friction syndrome? Journal of Science and Medicine in Sport. 2007;10:74-76.
9. Fetto J, Leali A, Moroz A. Evolution of the Koch model of the biomechanics of the hip: clinical perspective. Journal of orthopaedic science. 2002;7:724-730.
10. Fredericson M, Wolf C. Iliotibial band syndrome in runners: innovations in treatment. Sports medicine. 2005;35:451-459.
11. Gabbett TJ. The training-injury prevention paradox: should athletes be training smarter and harder? Br J Sports Med. 2016;50:273-280.
12. Gabbett TJ, Kennelly S, Sheehan J, et al. If overuse injury is a ‘training load error’, should undertraining be viewed the same way? Br J Sports Med. 2016;
13. Haggerty M, Dickin DC, Popp J, Wang H. The influence of incline walking on joint mechanics. Gait & posture. 2014;39:1017-1021.
14. Hamill J, Miller R, Noehren B, Davis I. A prospective study of iliotibial band strain in runners. Clinical Biomechanics. 2008;23:1018-1025.
15. Heiderscheit BC, Chumanov ES, Michalski MP, Wille CM, Ryan MB. Effects of Step Rate Manipulation on Joint Mechanics during Running. Medicine & Science in Sports & Exercise. 2011;43:296-302.
16. Khan KM, Scott A. Mechanotherapy: how physical therapists’ prescription of exercise promotes tissue repair. British journal of sports medicine. 2009;43:247-252.
17. Koch JC. The laws of bone architecture. American Journal of Anatomy. 1917;21:177-298.
18. Meardon SA, Campbell S, Derrick TR. Step width alters iliotibial band strain during running. Sports Biomech. 2012;11:464-472.
19. Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. British Journal of Sports Medicine. 2010;45:691-696.
20. Reiman MP, Bolgla LA, Loudon JK. A literature review of studies evaluating gluteus maximus and gluteus medius activation during rehabilitation exercises. Physiother Theory Pract. 2012;28:257-268.
21. Smith BE, Hendrick P, Bateman M, et al. Musculoskeletal pain and exercise—challenging existing paradigms and introducing new. Br J Sports Med. 2018;bjsports-2017-098983.
22. Wiewelhove T, Döweling A, Schneider C, et al. A meta-analysis of the effects of foam rolling on performance and recovery. Frontiers in physiology. 2019;10:376.
23. Willy R, Meardon S, Schmidt A, Blaylock N, Hadding S, Willson J. Changes in tibiofemoral contact forces during running in response to in-field gait retraining Journal of sports sciences. 2016;34:1602-1611.
24. Willy RW, Buchenic L, Rogacki K, Ackerman J, Schmidt A, Willson J. In-field gait retraining and mobile monitoring to address running biomechanics associated with tibial stress fracture. Scandinavian journal of medicine & science in sports. 2016;26:197-205.
25. Willy RW, Davis IS. The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. J Orthop Sports Phys Ther. 2011;41:625-632.
26. Willy RW, Meira EP. Current Concepts in Biomechanical Interventions for Patellofemoral Pain. Int J Sports Phys Ther. 2016;11:877-890.
27. Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin Biomech 2012;27:1045-1051.





