Picture yourself starting an exercise routine or going for a walk with your family. Your muscles warm up, your breathing picks up, and, without you really noticing, your body taps into its energy reserves.
Moving—and living, in general—is something most people don’t have to think about too much. Have you ever thought of the role of blood sugar (aka glucose) in this process?
For most of us, we don’t need to think about how our body will feel after we work out or how much sugar we need to start our day—our body manages on its own. So, how does your body maintain the delicate balance of glucose to keep you strong and energised? That is what we will be talking about in this blog. Why? Because understanding the relationship between physical activity and blood sugar can provide valuable insight for enhancing your fitness and overall health.

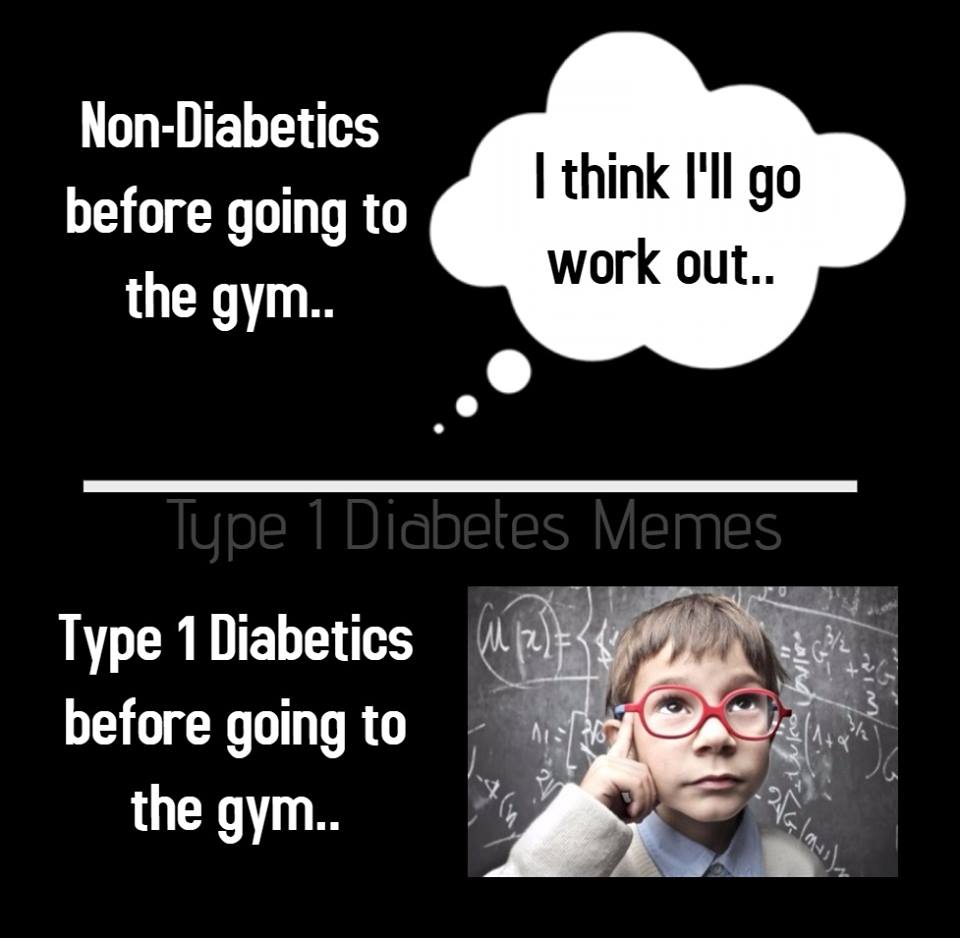
#image_title
What Happens?
Our body needs energy to function. Glucose is the main sugar in your blood that provides this energy for your body to think and move. It’s like fuel for your cells, keeping everything running smoothly and giving you the energy you need throughout the day. When your blood glucose levels are too low, you may experience fatigue, mental fog, and an unhappy mood. On the other hand, prolonged high levels of blood pressure can damage your blood vessels, which may harm your heart, eyes, and other organs that rely on a steady blood supply.
The pancreas, along with the hormones insulin and glucagon, helps to maintain the delicate balance between excessive and insufficient glucose levels. After consuming food, when blood glucose levels rise, the pancreas releases insulin, allowing glucose to enter the cells. More glucose in your cells means less in your blood, and once again, balance is restored. Excess glucose is converted into glycogen and stored in the liver and muscles for future use, such as between meals or during physical activity. If blood glucose levels drop too low, the pancreas releases another hormone called glucagon, which signals the liver to release stored glucose back into the bloodstream.
When your body loses its ability to manage these functions, it either produces insufficient insulin or cannot effectively use the insulin it does produce (known as insulin resistance). This results in persistently high blood glucose levels, which can lead to a range of serious health issues. Over time, persistent high glucose levels can damage blood vessels and nerves, potentially causing complications like heart disease, kidney failure, vision issues, and neuropathy. Additionally, this inability to regulate blood glucose levels can leave the body's cells without the energy they need, which can cause immediate symptoms such as dizziness, confusion, weakness, and even loss of consciousness, which can be dangerous if not promptly treated.
So Why is Exercise Good?
During exercise, blood glucose levels experience both short-term and long-term changes. In the short term, physical activity causes muscles to consume more glucose for energy, which reduces blood sugar levels—a beneficial effect for those with high blood sugar. Additionally, regular exercise enhances the body's sensitivity to insulin, enabling cells to absorb glucose more efficiently. This increased insulin sensitivity can last for several hours and up to 48 hours following exercise.
Regular exercise leads to lasting improvements in blood glucose control by enhancing insulin sensitivity, making it easier for the body to regulate blood sugar levels. This reduces the risk of developing insulin resistance and type 2 diabetes. Consistent physical activity also aids in weight management, reduces body fat, and increases muscle mass, all contributing to more stable blood glucose levels. Exercise helps the body use insulin more effectively and increases glucose uptake by muscles, which lowers blood sugar levels and boosts overall metabolic health. Additionally, it enhances cardiovascular health, making exercise essential for managing and preventing diabetes and other chronic diseases associated with poor blood sugar management (Thyfault & Bergouignan, 2020).
I Have Diabetes? Isn't Exercise Risky for me?
Exercise aids in better blood sugar management, even if you have insulin issues. It enhances your muscles' ability to utilise glucose immediately after exercise and increases your body’s insulin sensitivity for up to 48 hours afterward (Sylow et al., 2017).
When you have diabetes, your body can’t regulate glucose levels effectively. Physical activity can cause blood sugar to drop too low (hypoglycemia), especially if you are using insulin or certain diabetes medications. This can lead to symptoms like dizziness, confusion or fainting. On the other hand, intense or prolonged periods of exercise can sometimes cause your blood sugar to spike (hyperglycaemia), which can have some serious long-term effects on your blood vessels if it occurs frequently. Additionally, individuals with diabetes should be cautious of foot injuries or sores, as they may have reduced sensation and slower healing. If you have diabetes (type 1 or type 2), pre-diabetes, or a family history of diabetes, it is essential to consult with your GP and other healthcare professionals, such as exercise physiologists and dietitians, to develop a safe and effective exercise and nutrition plan
References:
Thyfault, J.P., Bergouignan, A. Exercise and metabolic health: beyond skeletal muscle. Diabetologia 63, 1464–1474 (2020). https://doi.org/10.1007/s00125-020-05177-6
Sylow, L., Kleinert, M., Richter, E. et al. Exercise-stimulated glucose uptake — regulation and implications for glycaemic control. Nat Rev Endocrinol 13, 133–148 (2017). https://doi.org/10.1038/nrendo.2016.162
Images Provided By:
BBC. (2024). A guide to percentages. BBC Bitesize. https://www.bbc.co.uk/bitesize/guides/z3gxb82/revision/7 and @t1diabetesmemes





